Our Services
Vitreoretinal Procedures
Pars Plana Vitrectomy (PPV)
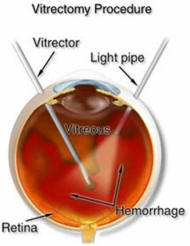
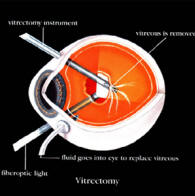
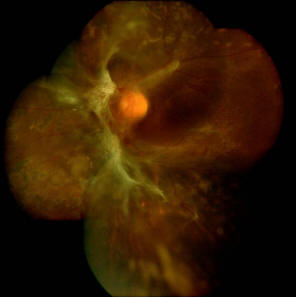
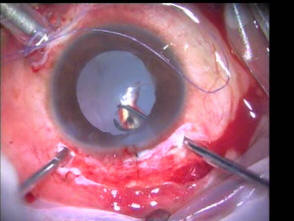
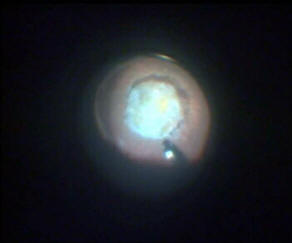
Pars Plana Vitrectomy surgery (PPV) or vitrectomy surgery is a form of surgery that treat disorders of the retina and vitreous. During this procedure, the vitreous is removed and usually replaced with a balance salt solution. Depending on the need for the surgery, the vitreous may also be replaced by either Gas, Silicone oil or a high density Silicone oil. The whole procedure may take between 30 to 90 minutes.
The term pars plana, implies that the surgery is performed in the deeper parts of the eyeball i.e behind the crystalline lens.
Together with PPV, other procedures may be performed as the need arises. Such procedures are:
When is Vitrectomy surgery indicated?
PPV is indicated in the following cases:
How is PPV performed?
Pars Plana Vitrectomy is a surgical procedure that is usually performed under local anaesthesia. In some severe cases, general anaesthesia may also be needed.
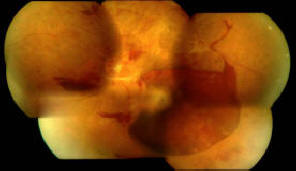
During the procedure, microsurgical instruments will be inserted into the eyeball via 3 small incisions (measuring about 2-3mm) that is made through the sclera (white of the eye). A number of instruments may be used during the procedure to removed the vitreous gel and any scar tissues that may have formed on the retinal surfaces. A laser probe can also be inserted during the procedure.
Depending on the complexity of the cases, other procedures may be combined with the PPV. Theses includes scleral buckling, cryopexy, and endotamponades (eg Silicone oil or gases).The entire surgery may take up between 45 minutes to 2 hours to complete.
Visual Outcomes
The visual outcomes following a PPV is largely depended on the severity and complexity of the case. If your eye problem caused permanent damage to your retina before the vitrectomy, then the improvement following surgery may not be great. Surgery is sometimes performed to save the eye only, rather than to achieve an improvement in vision.
Vitreoretinal Procedures
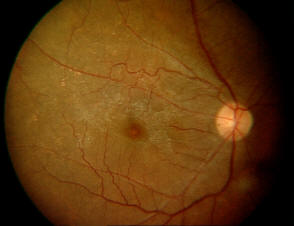
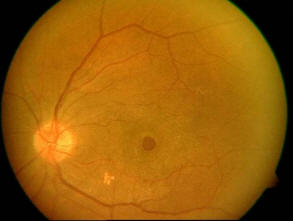
Age Related Macular Degeneration (ARMD)
Drag the bar to see how's ARMD patient see?
ARMD is condition that can occur in individuals above the age of 50 years. It tends to occur bilaterally but can affect only one eye initially. It is the leading cause of irreversible visual loss in the industrialized world and in Asia it is fast becoming a major cause of irreversible blindness. ARMD is condition that can occur in individuals above the age of 50 years. It tends to occur bilaterally but can affect only one eye initially. It is the leading cause of irreversible visual loss in the industrialized world and in Asia it is fast becoming a major cause of irreversible blindness.
What causes it?
Macular degeneration is caused by hardening of the arteries that nourish the retina. This deprives the sensitive retinal tissue of oxygen and nutrients that it needs to function and thrive. As a result central vision deteriorates. The central portion of the human retina contains a yellow pigment called the macular pigment. This pigment helps protect the sensitive receptors in the retina, particularly from the potentially harmful effects of blue light. The density of the pigment has been shown to be linked to diet and can be reduced in those who smoke.
The macula is the part of the retina that allows the eye to see fine details at the center of the field of vision. Degeneration results from a partial breakdown of the retinal pigment epithelium (RPE).
The RPE is the insulating layer between the retina and the choroid (the layer of blood vessels behind the retina). The RPE acts as a selective filter to determine what nutrients reach the retina from the choroid. Many components of blood are harmful to the retina and are kept away from the retina by normal RPE.
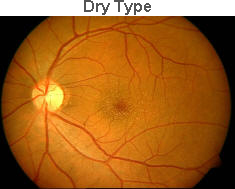
Breakdown of the RPE interferes with the metabolism of the retina, causing thinning of the retina (the "dry" phase of macular degeneration). These harmful elements may also promote new blood vessel formation and fluid leakage (the "wet" phase of macular degeneration).
This disorder results in the loss of central vision only -- peripheral fields are always maintained. Although loss of ability to read and drive may be caused by macular degeneration, the disease does not lead to complete blindness.
Types of ARMD
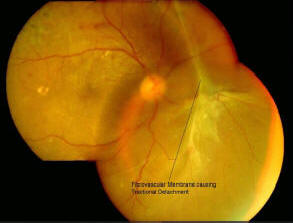
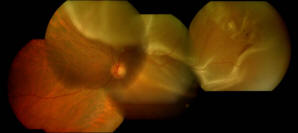
There are two main types of ARMD: the "dry" form and the "wet" form, based on the absence or the presence of abnormal growth of blood vessels under the retina known as Choroidal Neovascular Membrane. Most people with ARMD have the dry form.
Currently there is no proven treatment for the dry type, but the loss of vision tends to be milder and the disease progression is rather slow.
Approximately 10-15% of patients with ARMD have the wet form, where there is a growth of abnormal blood vessels under the retina, which can cause leakage, bleeding, and scarring, resulting in more rapid and severe vision loss. About 80% of severe vision loss is due to the wet form as compared to 20% due to the dry form.
The wet form can manifest in two types: classic or occult. Over 70% of patients with the wet form have the occult type

What happens to Vision ?
Some people with macular degeneration notice that straight lines in a landscape - such as telegraph poles, the sides of buildings or streets, appear wavy. Other symptoms include blurring of type or a page of print, with dark or empty spaces that may block the centre of the field of vision.
This is an example of what a patient with advanced macular degeneration might see:
Straight lines may become distorted
The central part of the visual field may be missing
Reading may become very difficult
Fortunately, macular degeneration rarely results in complete blindness since peripheral vision is usually unaffected. Although activities that require sharp vision such as reading, sewing or driving can be difficult, most people maintain their independence and should be able to get around outside and perform most household duties.
There is (currently) no known cure, but there are many indications that a good diet and healthy life style (particularly not smoking) will considerably reduce the chance of suffering from ARMD.
It is possible to carry out a simple test, to see if you might be suffering already without even knowing about it. In the early stages vision loss is only small and the brain cleverly covers up the defects so you don't notice. The AMSLER grid is a simple visual test that you can carry out on yourself in a few minutes
Instructions for using the Amsler grid
How to reduce the risks for ARMD?
1) Diet:
2) General Health:
How do we treat ARMD?
There is as yet no outright cure for macular degeneration, but some treatments may delay its progression or even improve vision. These include:
Thermal Laser Photocoagulation
The benefit of this treatment is that it can prevent further degeneration of the macula. However, the laser treatment can damage healthy macula cells meaning that you might lose a little sight to save a lot. Laser treatment is only useful in about 10 per cent of people with wet AMD and this always where people have reported their symptoms early.
Transpupillary Thermoplasty (TTT)
It involves shining a laser light of low intensity and at a specific wavelength onto the affected area. It does not damage the overlying healthy retina and only affects the abnormal vessels in the Wet AMD.
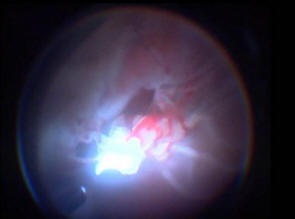
Photodynamic Therapy (PDT)
With PDT, a light-sensitive dye (Visudyne) is injected into the bloodstream and is transported to the retina at the back of the eye. This chemical highlights the blood vessels that are growing abnormally. A low energy or 'cold' laser beam is then shone onto the macula. This makes the chemical react and destroy the leaking blood vessels without damaging the healthy tissue around the affected area in the back of the eye. More than one treatment is usually required. PDT is unsuitable for long-established wet AMD and cannot restore sight that has already been damaged by macular degeneration. PDT cannot be used to treat dry AMD.
Anti Vascular Endothelial Growth Factor (VEGF)
VEGF has been shown to be important in the formation of the new vessels in the Wet type ARMD. The most recent development in the treatment of ARMD is the availability of Anti VEGF's. These drugs inhibit the role of VEGF in the formation of new vessels. It is injected directly into the eye with a small needle. This procedure is called Intravitreal Injection and is done in the clinic under topical anaesthesia. Anti VEGF's has been shown to be able to treat all forms of the Wet type ARMD, with some good visual recovery. It is however, necessary to have repeated 4-6 weekly injections for about 3-4 month. Further re treatments may be necessary depending on individual cases.
Will my vision return to normal after treatment?
As stated earlier, there are no cures for ARMD at this moment. All the treatment options discussed are designed to preserve whatever vision this is left. However, some patients do gain better visual improvement after treatment depending on the severity of their lesions.
Vitreoretinal Procedures
Eye Angiography
What is an angiogram?
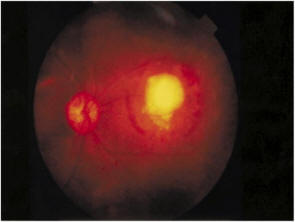
An angiogram is a procedure used in Ophthalmology to photograph the blood vessels of the retina. It involves inserting a needle into a vein, usually in the arm or back of the hand and injecting a diagnostic dye. Photographs of the retina are taken as the dye circulates through the bloodstream. Your Ophthalmologist may require this test to diagnose or monitor your retinal condition.
Are there any medical conditions or medications that may affect the procedure?
Please inform your Ophthalmologist if you suffer from any condition related to the heart, lungs or kidneys. These conditions do not exclude you from being able to have a fluorescein angiogram but your Ophthalmologist needs to be aware of such conditions.
Your Ophthalmologist should also be aware of your allergies and any medications you are taking.
What are the risks?
The risks associated with injection of fluorescein are low.
The most common side effect is nausea. If you do experience nausea it will occur during first 1-2 minutes after the dye is injected. Please inform the Nurse performing the procedure and she will be able to give you an alcohol swab to sniff which will help relieve the nausea. It normally only lasts 10-30 seconds. In rare cases vomiting may accompany the nausea.
Other adverse reactions include headache, hypotension (low blood pressure), fainting, gastric upset, convulsions, and intense lower back pain. Please inform the Nurse if you experience any of these reactions.
In rare cases patients may suffer an allergic reaction. If the reaction is mild you may break out in hives and feel itchy. In a more severe reaction anaphylaxis and respiratory/cardiac arrest may occur. Although the incidence of this type of reaction is extremely rare our staff are trained in resuscitation and a fully stocked emergency kit is located in each room where the procedure is performed.
As with any intravenous injection there is a small risk that the dye may leak into the tissue rather than being injected into the vein. If this does occur you may experience a burning sensation as the dye is injected and the injection site may be yellow and tender for the next few days. A cold pack may ease the pain and swelling. By drinking lots of water 1-2 days prior to the procedure you will minimize the risk of extravasation (leakage of dye into body tissue).
Vitreoretinal Procedures
Eye Angiography
What is an angiogram?
An angiogram is a procedure used in Ophthalmology to photograph the blood vessels of the retina. It involves inserting a needle into a vein, usually in the arm or back of the hand and injecting a diagnostic dye. Photographs of the retina are taken as the dye circulates through the bloodstream. Your Ophthalmologist may require this test to diagnose or monitor your retinal condition.
Are there any medical conditions or medications that may affect the procedure?
Please inform your Ophthalmologist if you suffer from any condition related to the heart, lungs or kidneys. These conditions do not exclude you from being able to have a fluorescein angiogram but your Ophthalmologist needs to be aware of such conditions.
Your Ophthalmologist should also be aware of your allergies and any medications you are taking.
What are the risks?
The risks associated with injection of fluorescein are low.
The most common side effect is nausea. If you do experience nausea it will occur during first 1-2 minutes after the dye is injected. Please inform the Nurse performing the procedure and she will be able to give you an alcohol swab to sniff which will help relieve the nausea. It normally only lasts 10-30 seconds. In rare cases vomiting may accompany the nausea.
Other adverse reactions include headache, hypotension (low blood pressure), fainting, gastric upset, convulsions, and intense lower back pain. Please inform the Nurse if you experience any of these reactions.
In rare cases patients may suffer an allergic reaction. If the reaction is mild you may break out in hives and feel itchy. In a more severe reaction anaphylaxis and respiratory/cardiac arrest may occur. Although the incidence of this type of reaction is extremely rare our staff are trained in resuscitation and a fully stocked emergency kit is located in each room where the procedure is performed.
As with any intravenous injection there is a small risk that the dye may leak into the tissue rather than being injected into the vein. If this does occur you may experience a burning sensation as the dye is injected and the injection site may be yellow and tender for the next few days. A cold pack may ease the pain and swelling. By drinking lots of water 1-2 days prior to the procedure you will minimize the risk of extravasation (leakage of dye into body tissue).